Resources
CODING & DOCUMENTATION
EDUCATION & EVENTS
ENROLLMENT & CREDENTIALING
 FORMS & MANUALS
FORMS & MANUALS
HEALTHCARE INFORMATION & TECHNOLOGY
 PATIENT HEALTH
PATIENT HEALTH
PHARMACY
 POLICIES & GUIDELINES
POLICIES & GUIDELINES
PRE-SERVICE REVIEW
 PROGRAMS & INITIATIVES
PROGRAMS & INITIATIVES
 PROVIDER NETWORKS & SPECIALTIES
PROVIDER NETWORKS & SPECIALTIES
Recredentialing
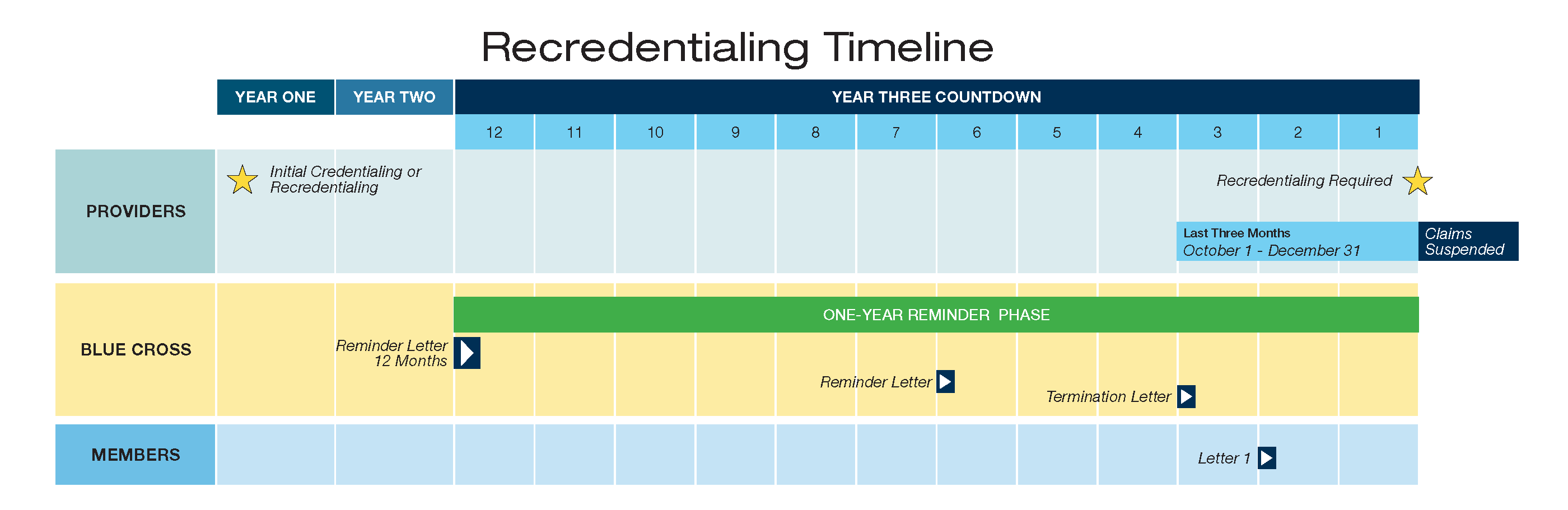
Contracted providers must be recredentialed with Blue Cross within three years to continue participation in our provider network(s). The chart below shows a sample of this three-year process, including our multiple efforts to reach out to providers during the one-year reminder phase prior to claims suspension, required member notifications, and termination from our network(s).
Blue Cross uses CAQH® ProView™ to streamline the credentialing process. If you are:
- An Existing ProView user - You are required to confirm the given data once every four months. Blue Cross will obtain your updated information from the ProView™ database and complete the recredentialing process.
- Not currently registered with ProView - You may self-register, complete the application, and upload credentialing documentation. Blue Cross will access the ProView™ database to obtain your information and complete the recredentialing process.
We encourage all providers to use ProView to experience firsthand how administrative burdens will be reduced. Please visit https://proview.caqh.org/ for more information.
Recredentialing Documentation
There are several required documents that you must submit for recredentialing. Print this checklist to track your progress throughout the recredentialing process and ensure that all necessary documents/forms are submitted. These items from the checklist can be uploaded to ProView and accessed by Blue Cross:
- Network Interest Form
- Current Professional State License
- Current Alabama Controlled Substance (ACSS) Certificate
- Federal DEA Certificate
- Evidence of Current Individual Professional Malpractice Liability Insurance (Domestic Carrier Required)
- Hospital Data Form
- Complete work and education history for the past three years, including explanations of any malpractice suits or issues
Providers who do not participate with ProView will be required to complete the Recredentialing Verification Form. All requested documentation must be submitted with this form to Blue Cross by:
- Fax: Attn: Credentialing 1-205-220-9545
- Mail: Blue Cross and Blue Shield of Alabama, Attn: Credentialing/Provider Data, P. O. Box 362142, Birmingham, AL 35236-2142
- Email: recredappl@bcbsal.org
Failure to complete the recredentialing process may result in termination from our provider networks.
Practitioner Rights
Requirements for Updating Provider Directory Information
CAQH is solely responsible for its products and services, including ProView.
