The Blue High Performance Network® (BlueHPN®) is a national Blue Cross and Blue Shield network. Providers have been specifically selected to participate in this new network because of their commitment to providing quality and affordable care to patients.
Important: Review the list of providers and hospitals designated for the BlueHPN.
Note: Review information about our Individual Exclusive Provider Organizations (EPO) Plans, which use the BlueHPN
|
Effective January 1, 2025, the BlueHPN will only include specialists who use in-network facilities for services. This means that many specialists, including but not limited to those based at University of Alabama at Birmingham (UAB) Hospital, will no longer be in network.
UAB’s planned acquisition of St. Vincent’s Health System is expected to result in renaming the Ascension St. Vincent’s facilities to “UAB St. Vincent’s.” Please note that St. Vincent’s hospitals and related physicians practicing at its facilities will remain in the BlueHPN.
|
How does the BlueHPN work?
BlueHPN is a comprehensive network that includes a full range of providers including primary care physicians, ancillary providers, specialists, hospitals and more. In Alabama, this network focuses on the Birmingham area. Only certain healthcare providers meet requirements to be part of this network. Not all healthcare providers are included in this network.
Providers have been automatically selected to be part of this new network. Review the list of providers and hospitals designated for the BlueHPN. There is no process for providers to apply to participate in this network. Providers who have been designated for this network do not have to take any action. More information is available on our BlueHPN FAQ webpage.
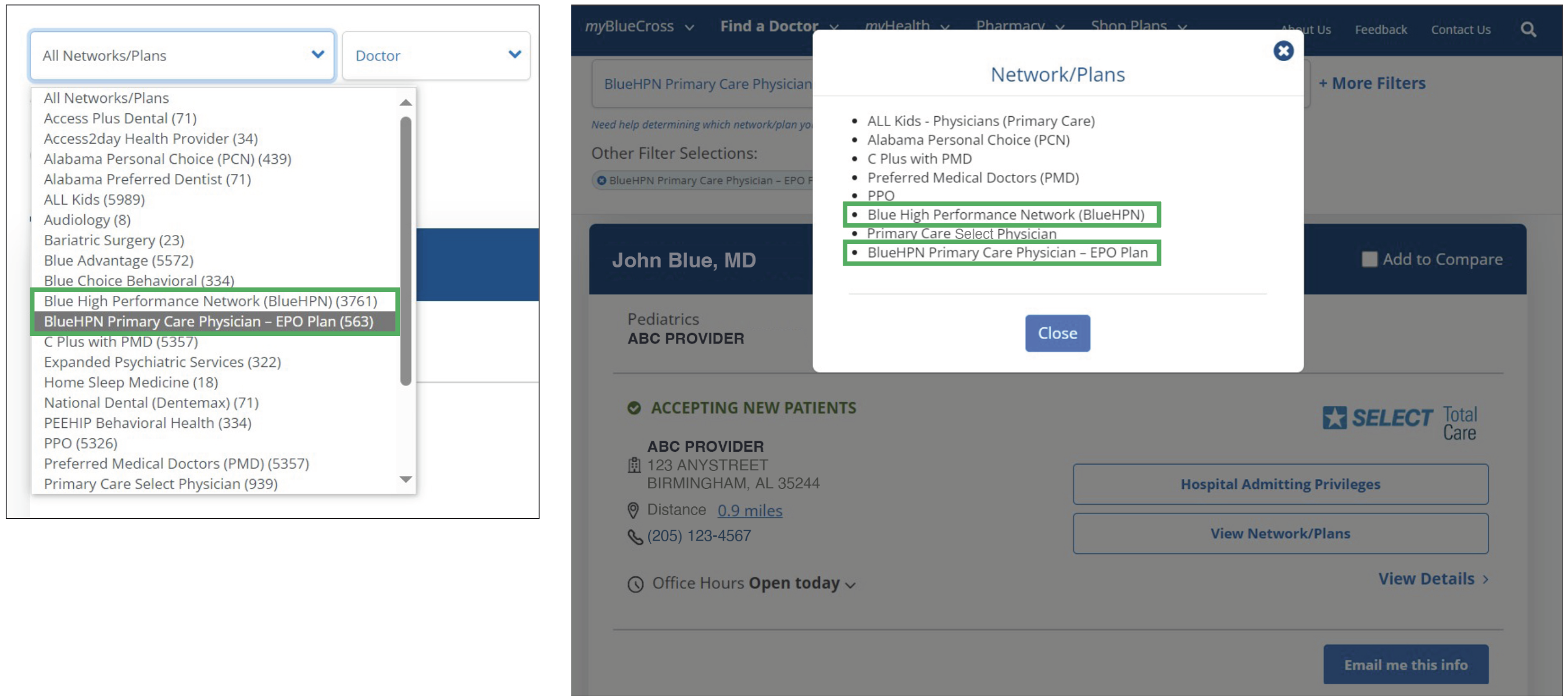
It's important that patients with this benefit plan receive care from BlueHPN healthcare providers to ensure they receive maximum benefits. Generally, services by non-BlueHPN providers are not covered. (Note: Effective January 1, 2024, urgent care and behavioral health services [mental health and substance abuse] no longer require designations or referrals for coverage.) Providers and patients can use our Find A Doctor tool to identify BlueHPN healthcare providers.
How can you identify patients in the BlueHPN?
BlueHPN patients can be identified by looking at their Blue Cross member ID card. "Blue High Performance Network" will be prominently displayed on the front of the ID card, along with an empty suitcase logo to help signify that their benefits are not portable like our traditional PPO plans. Generally, Individual EPO plan members have only coverage outside of the Birmingham MSA for urgent and emergent services:
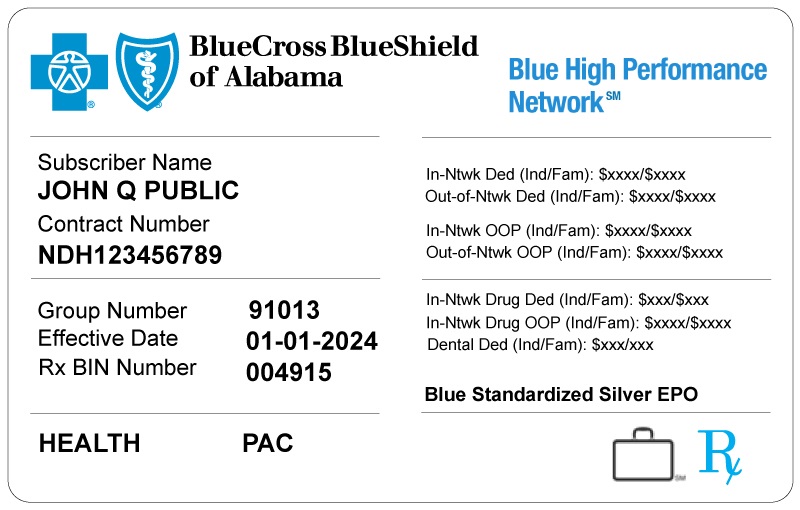
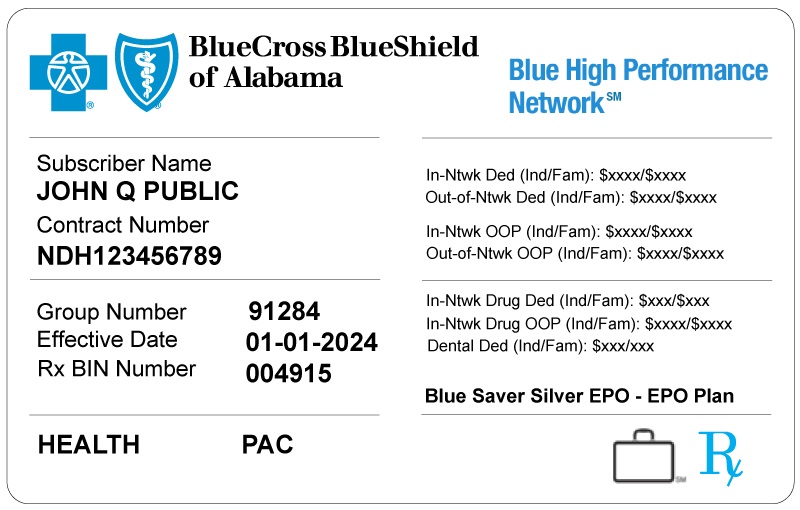
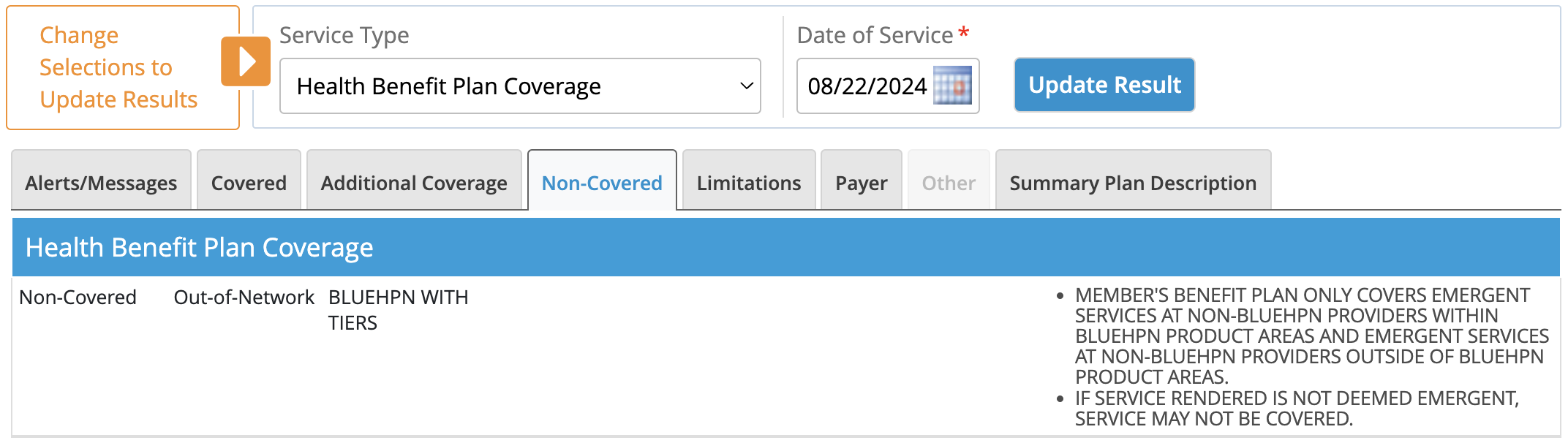
You can also determine if your patient is enrolled in this plan by checking eligibility and benefits, as shown in the image below.
What to Look for in ProviderAccess Eligibility and Benefits
Here are examples showing what you can expect to see for patients who are part of this new network:
On the “Covered” tab, providers will always see “Exclusive Provider Organization” along with either “HPN WITH TIERS” or “HPN WITHOUT TIERS” depending on the patient’s benefit structure.
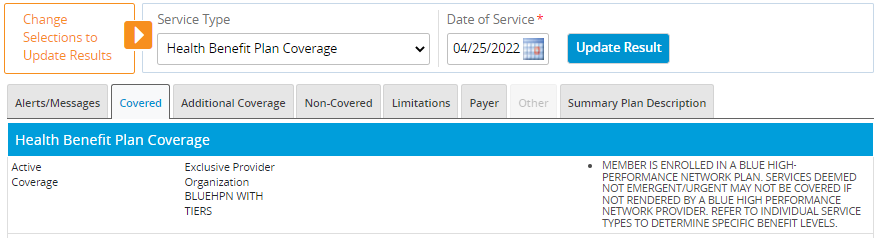
BlueHPN details and verbiage will vary depending on the patient’s benefit structure.

On the “Non-Covered” tab, providers will again either see “HPN WITH TIERS” or “HPN WITHOUT TIERS” along with the message shown on the right.
If you have questions, call Provider Networks at 1-866-904-4130.
 FORMS & MANUALS
FORMS & MANUALS
 PATIENT HEALTH
PATIENT HEALTH
 POLICIES & GUIDELINES
POLICIES & GUIDELINES
 PROGRAMS & INITIATIVES
PROGRAMS & INITIATIVES
 Advanced Practice Providers
Advanced Practice Providers