Medical Record Requests
Blue Cross and Blue Shield of Alabama routinely requires the submission of clinical information for the following:
- Unlisted codes
- Claims with the modifier 22
- Claims requiring review for medical necessity, including services or procedures for which Blue Cross has issued a coverage statement, coverage guidelines or a stated medical policy
- Potentially cosmetic claims
- Claims that are investigational in nature
Clinical information may also be required for claims that include services listed as contract exclusions under a member's contract, services which require precertification and services under review for potential fraud or abuse.
Medical Record Documentation
For additional information about medical record documentation, view our Medical Records Documentation webpage.
Medical Record Processing and Payments
Blue Cross and Blue Shield of Alabama uses electronic funds transfer (EFT) for medical records payments to copy service vendors and providers.
Reminders Regarding Medical Records Processing and Payments
- Payments to providers and medical records copy service vendors are made weekly.
- Blue Cross pays medical records copy service vendors at the same rates we reimburse providers for medical records, regardless of the amount billed. We will not pay late fees or interest charges.
- EFT is available for both providers and their vendors. Providers will receive reimbursement to the same account on file as their claims reimbursement. If a provider would like to sign up for EFT, log in to ProviderAccess, hover over Payment & Refund, and select Direct Deposits/EFT Registration. Vendors can contact Treasury Operations at 205-220-4745 or email provideraccountingeft@bcbsal.org for EFT signup information.
- Blue Cross will pay one search fee ($5) per request, plus a per-page allowance for each page submitted. An allowance for postage will be added for records received via mail.
- Certain medical records are not applicable for reimbursement, including those for Blue Advantage® (PPO), which can be identified with an MBG contract prefix as well as those for underwriting purposes.
- Reimbursement will not be made for records that are not requested by Blue Cross and Blue Shield of Alabama.
- Blue Cross does not currently access medical records requests online. Records must be mailed to the P.O. Box listed on the medical record request. Records can also be faxed. The fax information is listed on the Medical Request Letter.
- Blue Cross does not prepay for medical records. Payment will be made upon receipt of the medical records.
- It is the responsibility of the provider to communicate the request and payment system if a vendor is being used by the provider.
- The details for electronic payments can be found by logging in to ProviderAccess, hovering over Payment & Refund, and selecting Remittance – Miscellaneous Payments.
- A vendor should contact Ask-PSC@bcbsal.org when it has an unpaid invoice. The vendor should not contact us regarding paying late fees, interest charges, when payment is not what was expected, or payment for Blue Advantage medical records. The provider should contact their Network Consultant on behalf of their vendor if they see a high volume of incorrectly paid invoices.
Steps to Receive Payment
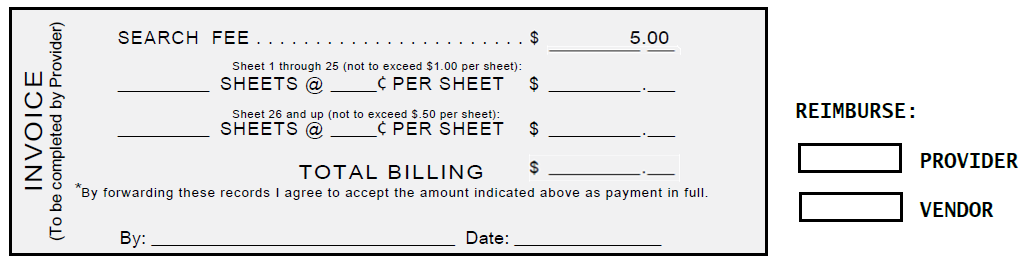
- Providers must request reimbursement for medical records by completing the invoice form (sample shown below) that is part of the request form. Reimbursement will not be made if a completed invoice is not received with the patient’s medical record.
- Indicate on the invoice whether payment should be made to the provider or the provider’s medical records copy service vendor.
Copy Service Vendor Payments
- Payments are mailed weekly.
- Medical record reimbursement rates are the same for providers and vendors.
- Bank statements will note the following for refunds: Medical Records-BCBSALMEDR.
- The medical records remittances state the following: Attention Medical Records Department.
 FORMS & MANUALS
FORMS & MANUALS
 PATIENT HEALTH
PATIENT HEALTH
 PROGRAMS & INITIATIVES
PROGRAMS & INITIATIVES
 PROVIDER NETWORKS & SPECIALTIES
PROVIDER NETWORKS & SPECIALTIES