Resources
CODING & DOCUMENTATION
EDUCATION & EVENTS
ENROLLMENT & CREDENTIALING
 FORMS & MANUALS
FORMS & MANUALS
HEALTHCARE INFORMATION & TECHNOLOGY
 PATIENT HEALTH
PATIENT HEALTH
PHARMACY
 POLICIES & GUIDELINES
POLICIES & GUIDELINES
PRE-SERVICE REVIEW
 PROGRAMS & INITIATIVES
PROGRAMS & INITIATIVES
 PROVIDER NETWORKS & SPECIALTIES
PROVIDER NETWORKS & SPECIALTIES
Patient Health Snapshot
Blue Cross offers the interactive Patient Health Snapshot (PHS) to help provide you with a complete picture of your patient’s health. The PHS gives you easy access to important patient health information, including:
- Gaps in care
- Chronic conditions and diagnoses
- Recently received healthcare
- Drug information
Access the Patient Health Snapshot from the drop-down menu under Patient & Claim. Refer to the PHS each time a patient comes into the office as gaps in care and diagnosis information often changes. In preparation for patient office visits, you can also print the traditional format PHS by clicking the blue “View/Print PHS” button in the upper-right corner of the application.
PHS Quick Reference Guide
With the exception of the Conditions/Diagnoses sections, the PHS displays information for a 12-month rolling period, not a calendar year. The Conditions/Diagnoses section displays information for the full prior year and the current year-to-date data.
Filter Options
You can view patient data for an individual patient or all patients in a medical group. To view data for all patients, choose the “All Medical Group Patients” tab. You will then have an option to sort the list of patients by choose the downward triangle to the right of each column. This enables you to filter the list by the number of gaps in care or potential conditions. You can also sort to view patients with a low, medium, high or very high risk of non-adherence with medications.
You can easily select patients from the list and then view and print that list by clicking the blue View/Print PHS button on the right-hand side.

Care Gaps – Non-Compliant or Compliant/Controlled (Data Lag: Up to 7 Days)
- See recommended screenings for the patient according to nationally endorsed quality metrics and how often they should be performed.
- If the patient is non-compliant on any of these screenings, consider performing or ordering the service to ensure the patient has no gaps in care.
- See coding guides on our Coding and Documentation webpage for help in closing gaps in care.
Recent Care (Data Lag: Up to One Month)
This section will indicate whether the patient has had a preventive visit or, for Blue Advantage® patients, an annual wellness visit in the current year. Recent care includes:
- Preventive Visit (Data Lag: Up to One Month)Annual Wellness Visit for Blue Advantage Patients (Data Lag: Up to One Month)
- ER Visits/Admissions/Readmissions*
*The emergency room/hospital utilization section on the PHS is unavailable at this time. We are making enhancements to provide the most up-to-date information. In the meantime, primary and urgent care providers can use Care Alerts to be notified in nearly real-time when an attributed patient has an emergency room visit or is admitted to or discharged from the hospital.
Conditions/Diagnoses* (Data Lag: Up to One Month)
This section includes diagnoses that map to a U.S. Department of Health and Human Services (HHS) Category Condition or, for Blue Advantage patients, diagnoses that map to a CMS Hierarchical Condition Category (HCC) received for the patient in the current or prior calendar year.
In addition to showing the diagnosis codes and descriptions, the Conditions/Diagnoses section of the Blue Advantage PHS will display the corresponding HCC code and description for each diagnosis. A flag will indicate if we received the condition from multiple sources and a column will indicate the source of the condition (i.e., Claim, Supplemental Data, HR360, HRA or AWV).
When viewing the PHS for a Blue Advantage patient, the diagnoses in this section will correspond directly with the Risk Recapture Rate incentive offered through the Blue Advantage Primary Care Incentive Program.
*Sources of Data for Patient Conditions/Diagnoses: Information in this section includes data obtained from multiple sources – claims, internal or vendor medical record reviews, and health risk assessments. In cases where a diagnosis was coded as a result of an internal or vendor chart review, the “Provider” column on the PHS will be populated with the provider name (when available) or labeled as “Supplemental Data.” In the case of an in-home health risk assessment, the provider name will be populated with “HRA.”
Disputing Chronic Conditions – Blue Advantage Patients OnlyFrom April 1 - December 31, providers can dispute or resolve conditions listed on the Patient Health Snapshot (PHS). This process applies to Blue Advantage patients only. When to choose the Dispute or Resolve Conditions option:
Click the “Dispute or Resolve Conditions” button in the upper-right corner of the Conditions/Diagnoses section to begin this process. Use the "PHS Dispute/Resolved report" available on ProviderAccess to show you what Patient Health Snapshot (PHS) diagnosis codes have been disputed and resolved for your patients. The “PHS Dispute/Resolved report” refreshes with the most current data each time it runs, which may result in slower performance compared to other reports. Here are some key features:
Note: If multiple claims are submitted for the same diagnosis code, the dispute code may reappear on the PHS report. For more information on how to dispute or resolve diagnoses listed on the PHS, refer to the Blue Advantage Patient Health Snapshot Disputing or Resolving Chronic Conditions Guide. To access the report in ProviderAccess, select Profiles & Reports then click “Blue Advantage PHS Dispute/Resolved”. |

Medication Adherence – Blue Advantage Patients Only (Data Lag: Up to 30 Days)
This section shows information about your Blue Advantage patients’ medication adherence in three specific condition-related measures:
- Diabetes: Medication Adherence for Diabetes Medications
- Statins: Medication Adherence for Cholesterol
- RAS (Renin Angiotensin System Antagonists): Medication Adherence for Hypertension
Note: This section only populates data for your Blue Advantage patients.
The Medication Adherence section will be populated if your patient has a prescription that falls within one of these specific measures. You will see the most recently filled medication for the specific measure, as well as its last fill date. If the patient takes more than one medication in the specific measure listed, only the most recently filled medication will display. If there is no prescription that corresponds to a specific measure, that measure will not appear for that patient in this section.
Proportion of Days Covered (PDC): The PDC is calculated using the quantity and days’ supply values submitted on pharmacy claims for all drugs in the measure. It assesses how consistently a patient fills their medications for the time period measured. A PDC threshold of 80% is used to indicate adherence, meaning patients are considered adherent if they have filled their prescriptions for at least 80% of the days expected based off the days’ supply indicated on their prescription.
- Note: The PDC displayed is calculated using a rolling 12-month period (not year-to-date) to better reflect their long-term adherence, when available.

Recommended Action: Based on your patient’s medication usage, you may see some clinical suggestions to consider in the column titled “Recommended Action.” Click the action link to view the details about each response.
Note: Medications in this section are highlighted if there is a recommended action for the provider to consider.

Care Management Programs – (Data Lag: Up to 7 Days)
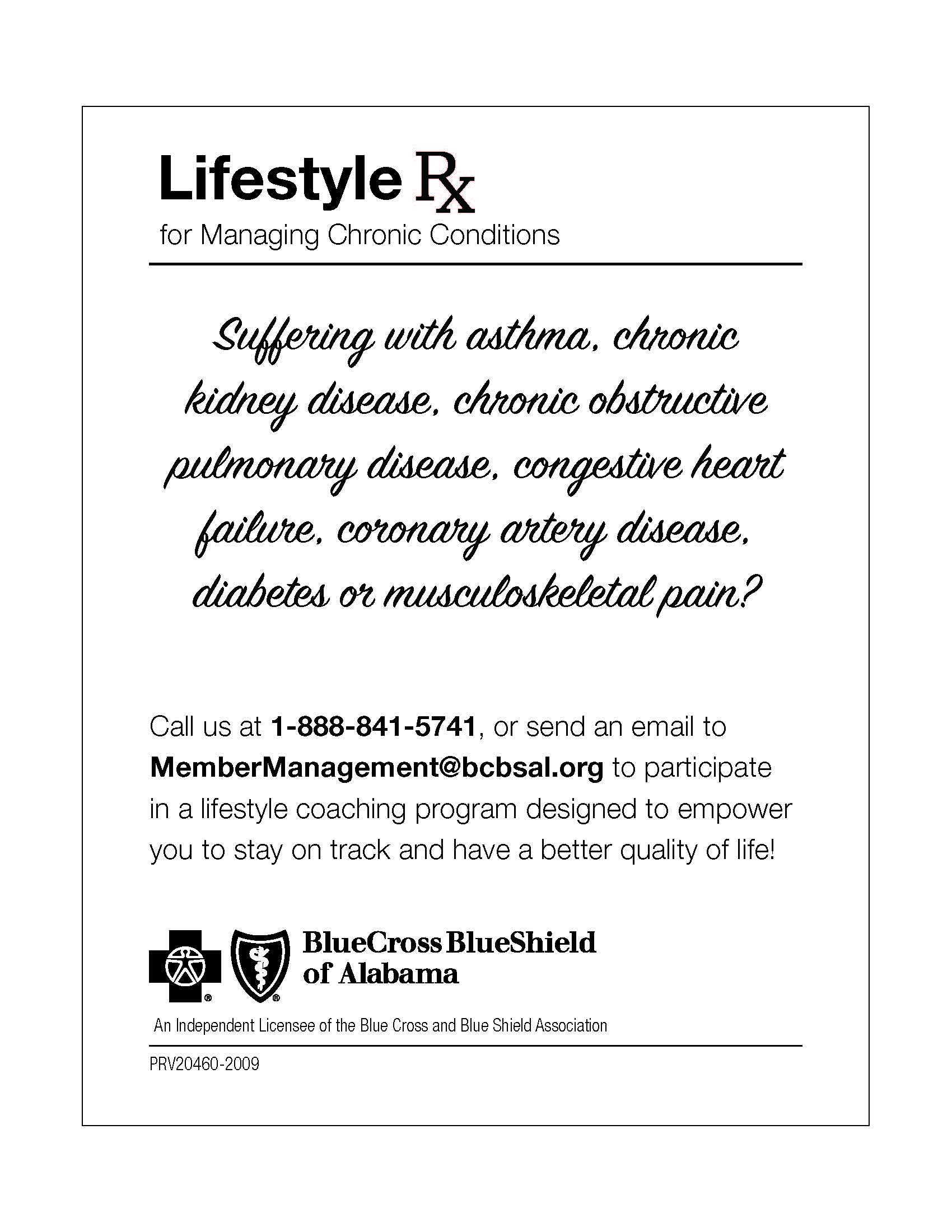
The Care Management Programs section displays information when your patients qualify for any of our health and clinical engagement programs, such as Baby Yourself, REACH Kidney Care, Chronic Condition Management, and Health Coaching. This section is available via a link in the upper-left corner below the patient's name.
If your patient is currently enrolled in a program or eligible for a program, the Care Management Programs link will be available. This section will display the available enrolled or eligible program(s) for your patient. The “Eligible” link next to a program will display a sample patient handout that explains the available program and how to enroll. Order these handouts through our Patient Handouts Request Form.